What is breast reconstruction?
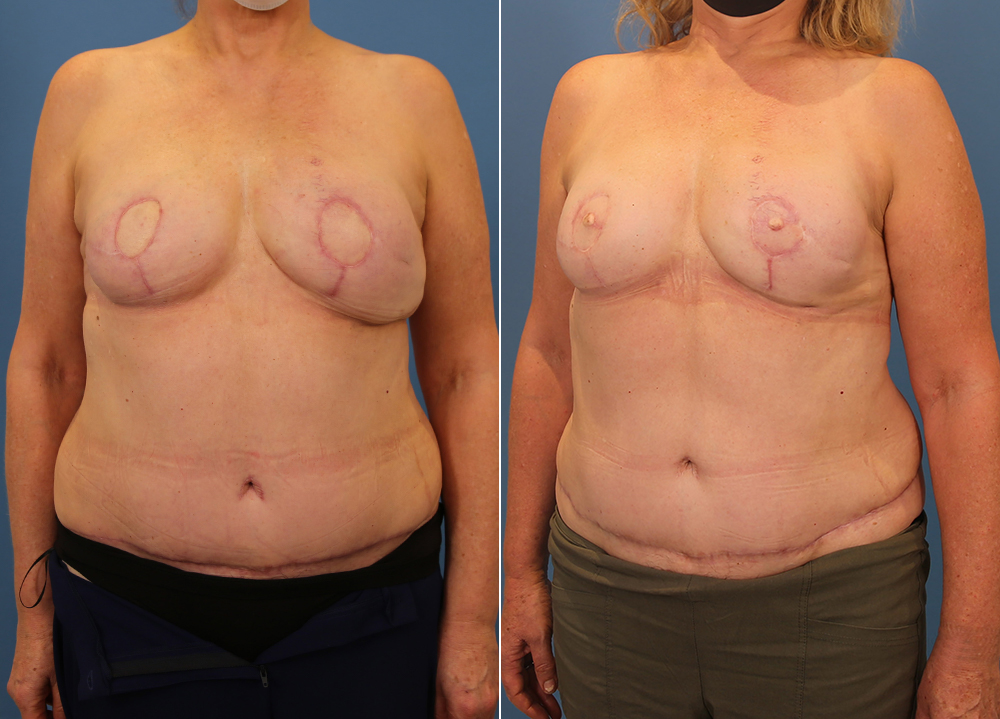
Breast reconstruction is surgery to make a new breast after removal of the breast or part of the breast. The aim is to make a breast of similar size and shape to your original breast.
This can be done either using an implant or from tissue (skin, muscle or fat) from another part of your body.
Depending on your treatment (if you have had a mastectomy due to breast cancer), breast reconstruction may be performed at the time of your mastectomy or at a later date.
After reconstruction surgery you might also wish to consider more surgery to:
- Create a new nipple (a nipple reconstruction)
- Change the shape of your other breast to match



DO YOU NEED BREAST RECONSTRUCTION FOLLOWING BREAST CANCER?
Breast reconstruction takes many varied forms but can be broadly divided into three main areas. Firstly, using your own tissue to make a breast (autologous reconstruction). Secondly, using predominantly an implant to make a breast (alloplastic reconstruction) and finally using a combination of both, i.e a hybrid breast reconstruction.
The treatment of breast cancer is also rapidly developing – it is still mostly divided into situations where the breast was reconstructed at the same time as the mastectomy (immediate) or after cancer treatment was finished (delayed). There are some newer variations, such as the treatment of gene mutation – positive patients (e.g. BRCA1 or 2) or reverse radiotherapy sequencing but the general process remains the same. i.e. treat the cancer first and then reconstruct the breast.
I am specifically known for performing autologous reconstructions and hybrid reconstructions. That is, using your own excess fat (mostly from the abdomen) to make you a new breast that will feel and respond like a normal breast would.
Reasons for breast reconstruction
MASTECTOMY
Mastectomy may be used to reduce the risk of breast cancer developing in women with a high risk of breast cancer. This is called preventative or prophylactic mastectomy. Mastectomy may also be used to treat breast cancer in women who have been diagnosed with the disease.
In this instance, breast reconstruction is surgery to rebuild a breast shape after mastectomy.
TUBEROUS BREAST DEFORMITY
Tuberous breast deformity is a recognised anatomical variation of the breast. It has three features that typify the complete condition that include:
- A short distance between the nipple and the crease under the breast.
- A typically larger areola, with the breast gland almost falling through the overlying skin looking puffy.
- The breast has usually less volume with wide spacing between the breasts.
MAJOR BREAST ASYMMETRY
There is degree of asymmetry between all breasts, but some patients have more than others. When that difference between your breasts is significant you may want to do something about it. Why? The reasons may range from self- all the way to practical concerns of being able to buy bras without difficulty. The first question that needs to be answered is this: What is the goal? Once we establish then it is usually a carefully planned process that means we aim towards the smaller breast, the larger breast or aim to change both breasts.
POORLY DEVELOPED BREASTS OR NIPPLE POSITION IRREGULARITIES
Most patients having breast augmentation have some elements but for some people there can be precious little skin or breast on the chest wall. An implant alone is usually the starting point and this is often augmented by techniques such as fat grafting.
If you have nipple position issues you will often require two stages to achieve your goals. One stage involves placing the implant and the second involves moving the nipple. Common sense should prevail here. Small differences between the nipples are common place and not worth the additional scars usually.
PIDGEON OR HOLLOW CHEST DEFORMITIES
The sternum and ribs can best be thought of as the foundation on which we build your new breasts. The main presentations tend to be a hollow chest deformity or the opposite phenomenon where the chest can appear excessively proud like the keel of a boat. Scoliosis and rib anomalies can also be present with both these conditions and will impact your final result and the approach to achieve your surgical goals.
Any skeletal or rib-based issue can be treated with cardiothoracic surgery, but this is usually reserved for the most extreme cases. Even then, surgery is rarely performed unless there are functional concerns at the same time. Careful choice of an appropriate implant with possible fat grafting can be extremely effective for this situation.
FREQUENTLY ASKED QUESTIONS ABOUT OUR BREAST RECONSTRUCTION PROCEDURES
If you have enough abdominal tissue then an autologous reconstruction using this tissue to make a breast will give you the best long-term aesthetic result. There are two main types of reconstructions that use this abdominal tissue. One is called a TRAM flap and the other is called a DIEP flap. The main difference between the operations is that the TRAM flap also takes your abdominal core muscle at the same time and the DIEP leaves the muscle behind.
If you have suitable blood vessels and anatomy, the DIEP flap has obvious benefits as your rectus abdominus muscle is not unnecessarily wasted. There are some people who simply do not have favorable anatomy for a DIEP flap and might require the TRAM flap instead.
My preference is always towards muscle preservation with a DIEP flap.
It is difficult to assign a cost to this kind of procedure on our website as there are many varied presentations and so many approaches that might be applicable to your situation. Some conditions are deemed medically required so private health insurance and Medicare can help, but our patient coordinators can help you assess your level of coverage. For more information please visit our pricing page by clicking here.
Breast reconstruction following a mastectomy for breast cancer is available in the public hospital system as well as through the private health system. It is considered a medical procedure, not cosmetic surgery. There is no charge to you for the procedure if you have your breast reconstruction through the public health system.
Most people will try to take a week off work and then go back to work after that.
Recovery can be thought of in two ways. Your aesthetic recovery can be seen no earlier than around 6 weeks for most patients but the final result where the breast is fully relaxed around the implant can take around 6 months.
Risks and complications of cosmetic surgery
Cosmetic surgery is still surgery and as such always has potential risks and complication. It is important for anyone considering cosmetic surgery to be well-informed and aware of the possible adverse outcomes. Dr Alex Phoon is a fully qualified Australian specialist plastic and cosmetic surgeon who operates with an experienced team in leading public and private hospitals in Sydney Australia.
In this article, we will dive into the various risks and complications associated with cosmetic surgery, providing insights into each aspect.
Scarring
One of the most common concerns among patients undergoing cosmetic surgery is the potential for scarring. While skilled surgeons strive to minimize scarring, it is an inevitable part of the healing process.
Read moreThe severity of scarring varies depending on the individual and the procedure performed. Certain factors, such as genetics and skin type, can also influence how prominent scars may be. However, it is worth noting that in many cases, scars fade over time and can be further improved through scar revision techniques.
Scarring is a natural part of the body’s healing process. When the skin is injured, whether through surgery or trauma, the body responds by forming new collagen fibres to repair the damage. This process can result in the formation of a scar, which is a visible mark on the skin that differs in texture and colour from the surrounding tissue.
There are different types of scars that can occur after cosmetic surgery. One common type is a hypertrophic scar, which is characterized by raised and thickened tissue. These scars may be red or pink in colour and can be itchy or uncomfortable. Another type of scar is a keloid, which is an overgrowth of scar tissue that extends beyond the boundaries of the original wound. Keloids are more common in individuals with darker skin tones and can be more challenging to treat.
Fortunately, advancements in surgical techniques and post-operative care have greatly improved the management of scars. Surgeons take great care in placing incisions in inconspicuous areas and using techniques to minimize tension on the wound, which can help reduce the risk of visible scarring. Additionally, patients are often advised to follow a specific scar care regimen, which may include keeping the incision site clean, applying silicone gel or sheets, and avoiding sun exposure.
In some cases, scar revision techniques may be recommended to further improve the appearance of scars. These techniques can include laser resurfacing, dermabrasion, or surgical excision. Laser resurfacing uses a laser to remove the top layers of the skin, promoting the growth of new, healthier skin cells. Dermabrasion involves using a rotating brush or diamond wheel to gently remove the outer layers of the skin, revealing smoother skin underneath. Surgical excision involves removing the scar tissue and rejoining the edges of the skin to create a more aesthetically pleasing scar.
It is important for patients to have realistic expectations when it comes to scarring. While surgeons strive to minimize scarring, it is impossible to eliminate it. However, with proper care and the use of scar revision techniques, the appearance of scars can be significantly improved. Patients should discuss their concerns and expectations with their surgeon prior to undergoing any cosmetic procedure to ensure they have a clear understanding of the potential for scarring and the available treatment options.
Infection
Infections are another risk associated with any surgical procedure, including cosmetic surgery. Despite stringent sterilization protocols followed by healthcare professionals, there is still a possibility of infection.
Read moreTo mitigate this risk, surgeons prescribe antibiotics pre- and post-surgery, adhere to aseptic techniques, and closely monitor patients for signs of infection. It is crucial for patients to follow their surgeon’s aftercare instructions to minimize the risk of infection.
When it comes to cosmetic surgery, infection is a concern that cannot be ignored. Surgical procedures, no matter how minor, create an entry point for bacteria and other microorganisms. Although healthcare professionals take every precaution to maintain a sterile environment, the human body is naturally teeming with bacteria, making it impossible to eliminate the risk entirely.
Fortunately, surgeons are aware of this risk and take proactive measures to minimize the chances of infection. One such measure is the prescription of antibiotics. Prior to surgery, patients are often given a course of antibiotics to help prevent any potential infection from taking hold. These antibiotics are carefully chosen based on the patient’s medical history and the specific procedure being performed.
Post-surgery, patients are usually required to continue taking antibiotics for a certain period. This helps to ensure that any bacteria that may have entered the body during the procedure are promptly eradicated. By adhering to the prescribed antibiotic regimen, patients can significantly reduce the risk of developing an infection.
In addition to antibiotics, surgeons also follow strict aseptic techniques during the surgical procedure itself. This involves maintaining a sterile environment, using sterile instruments and equipment, and wearing appropriate protective clothing, such as gloves and masks. These precautions help to minimize the introduction of bacteria into the surgical site, further reducing the risk of infection.
Despite these measures, it is important to note that infections can still occur. The human body is a complex system, and sometimes even the most stringent precautions cannot completely eliminate the risk. However, by closely monitoring patients for signs of infection, surgeons can detect and treat any potential infections early on, preventing them from becoming serious complications.
Patients also play a crucial role in minimizing the risk of infection. Following the surgeon’s aftercare instructions is of utmost importance. This may include keeping the surgical site clean and dry, avoiding certain activities or behaviours that could increase the risk of infection, and promptly reporting any signs of infection, such as redness, swelling, or discharge.
In conclusion, while the risk of infection is present in any surgical procedure, including cosmetic surgery, healthcare professionals take numerous precautions to minimize this risk. From prescribing antibiotics to following aseptic techniques, surgeons prioritize patient safety and strive to create the best possible outcome. However, it is essential for patients to actively participate in their own aftercare and follow the instructions provided by their surgeon to further reduce the risk of infection.
Pain
Pain and discomfort is a common experience following cosmetic surgery but can be mitigated with modern analgesic strategies.
Read moreThe extent of pain can vary depending on the procedure, the individual’s pain tolerance, and the body’s healing response. Surgeons typically prescribe pain medications to manage any discomfort during the recovery period. It is important for patients to communicate their pain levels with their healthcare providers, as proper pain management is crucial for a smooth recovery.
Undesirable cosmetic outcome
While cosmetic surgery aims to enhance aesthetics, there is always a risk of an undesirable cosmetic outcome.
Read moreFactors such as unrealistic expectations and the biological unpredictability of healing can contribute to suboptimal results. It is essential for patients to have open and honest discussions with their surgeons about their desired outcomes, potential limitations, and realistic expectations. This helps ensure that both parties are on the same page and reduces the chances of disappointment. Revision surgery might be an option should this be an issue.
Nerve damage
Another potential complication of cosmetic surgery is nerve damage.
Read moreSurgeons take great care to avoid damaging nerves during procedures, but it is not always possible to eliminate this risk entirely. Nerve damage can cause numbness, tingling, or loss of sensation in the operated area. In most cases, nerve function gradually improves, but it may take some time for complete resolution. Patients should be aware of this potential risk and discuss it with their surgeon before proceeding with the surgery.
Bruising and swelling
Bruising and swelling are common after cosmetic surgery, particularly in the early stages of recovery.
Read moreThese symptoms are part of the body’s natural response to trauma. Surgeons may recommend compression garments, elevation, and cold compresses to help minimize these effects. While bruising and swelling are temporary, they can cause discomfort and can affect the recovery timeline. Patience and adherence to post-operative guidelines can aid in reducing the duration and severity of these side effects.
Bleeding
Bleeding during or after surgery is a potential complication that can occur in any surgical procedure, including cosmetic surgery.
Read moreSurgeons take measures to control bleeding during the operation, but occasionally, some post-operative bleeding may occur. It is crucial for patients to inform their healthcare providers if they experience excessive bleeding or if they are unable to control bleeding with gentle pressure. Immediate medical attention is necessary to address this complication. If there is major bleeding, you might require a blood transfer or transfer to a hospital for additional treatment.
Seroma
A seroma is a pocket of fluid that can accumulate under the skin after surgery.
Read moreIt forms as a result of the body’s inflammatory response. Seromas are more common in larger surgical procedures and can lead to swelling and discomfort. Surgeons may drain seromas through aspiration or place drains to prevent their accumulation. A surgical drain can be used to minimise this risk. Close monitoring by healthcare providers is crucial to ensure the timely detection and management of seromas.
Anaesthetic complications
Although rare, complications related to anaesthesia can occur during cosmetic surgery.
Read moreAnaesthesia is administered to ensure patient comfort and safety during the procedure. Factors such as individual reactions, allergies, or underlying health conditions can increase the risk of complications. Anaesthetists are highly trained professionals who monitor patients closely throughout the surgery to minimize any potential risks.
Death
While the risk of death from cosmetic surgery is extremely low, it is essential to acknowledge that any surgical procedure carries inherent risks.
Read moreEvery effort is made to prioritize patient safety and ensure favourable outcomes. The preoperative assessment, careful surgical planning, and adherence to appropriate protocols help minimize this risk. Patients should discuss their specific concerns with their surgical team and feel confident in the expertise and experience of their chosen surgeon.
In conclusion, cosmetic surgery offers individuals an opportunity to enhance their appearance, but it is essential to recognize that it is not without its risks and complications. By understanding and discussing these potential outcomes with their surgeons, patients can make informed decisions and take necessary precautions to optimize their safety and overall surgical experience. With proper expectations, diligent aftercare, and open communication, the risks associated with cosmetic surgery can be minimized, and the goal of achieving desired aesthetic improvements can be realized.